Knee Surgery, Sports Traumatology, Arthroscopy ( IF 3.3 ) Pub Date : 2023-08-10 , DOI: 10.1007/s00167-023-07532-7 Tianshun Xie 1 , Maarten R Huizinga 2 , Inge van den Akker-Scheek 1 , Hugo C van der Veen 1 , Reinoud W Brouwer 2
|
Purpose
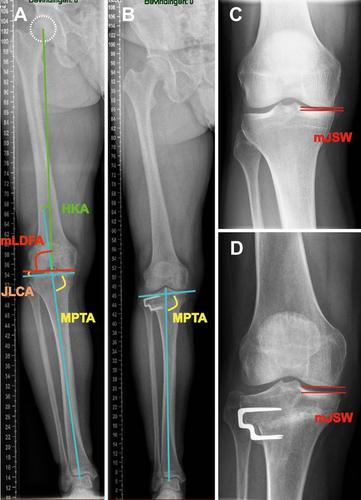
To analyze the association between change in knee joint line obliquity (KJLO) and patient-reported outcome, radiological progression of osteoarthritis, and surgical survival after lateral closing-wedge high tibial osteotomy (HTO).
Methods
A cohort of 180 patients treated in one single hospital with lateral closing-wedge HTO was examined. KJLO was defined by the medial proximal tibial angle (MPTA). To assess the association between KJLO and patient-reported outcome, radiological progression of osteoarthritis, and surgical survival, patient groups were defined: I, postoperative MPTA < 95.0°; II, postoperative MPTA ≥ 95.0°; A, MPTA change < 8.0°; B, MPTA change ≥ 8.0°. Propensity score matching was used for between-groups (I and II, A and B) covariates matching, including age, gender, preoperative lower limb alignment, preoperative medial joint space width (mJSW), preoperative Western Ontario and McMaster Universities osteoarthritis Index (WOMAC) score, wedge size, and postoperative follow-up time. Patient-reported outcome was assessed by the WOMAC questionnaire, radiological progression of osteoarthritis by mJSW and Kellgren–Lawrence (KL) grade progression (≥ 1) preoperatively and at follow-ups (> 2 years). Failure was defined as revision HTO or conversion to knee arthroplasty.
Results
After propensity score matching, groups I and II contained 58 pairs of patients and groups A and B contained 50 pairs. There were no significant differences in postoperative WOMAC score or surgical failure rate between groups I and II or between groups A and B (p > 0.05). However, the postoperative mJSW was significantly lower in group I than group II (3.2 ± 1.6 mm vs 3.9 ± 1.8 mm; p = 0.018) and in group A than group B (3.0 ± 1.7 mm vs 3.7 ± 1.5 mm; p = 0.040). KL grade progression rate was significantly higher in group I than group II (53.4% vs 29.3%; p = 0.008) and in group A than group B (56.0% vs 28.0%; p = 0.005).
Conclusion
Increased KJLO (postoperative MPTA ≥ 95.0°) or MPTA change ≥ 8.0° after lateral closing-wedge HTO does not adversely affect patient-reported outcome, radiological progression of osteoarthritis, or surgical survival at an average 5-year follow-up.
Level of evidence
III, retrospective cohort study.
中文翻译:

侧向闭合楔形胫骨高位截骨术后关节线倾斜不会对临床和放射学结果产生不利影响:一项 5 年随访研究
目的
分析膝关节线倾斜度 (KJLO) 的变化与患者报告的结果、骨关节炎的放射学进展以及外侧闭合楔形高位胫骨截骨术 (HTO) 后的手术生存率之间的关联。
方法
对在一家医院接受侧向闭合楔形 HTO 治疗的 180 名患者进行了队列检查。KJLO 由内侧近端胫骨角 (MPTA) 定义。为了评估 KJLO 与患者报告的结果、骨关节炎的放射学进展和手术生存之间的关联,患者组被定义为:I,术后 MPTA < 95.0°;II、术后MPTA≥95.0°;A、MPTA变化<8.0°;B、MPTA变化≥8.0°。倾向评分匹配用于组间(I和II、A和B)协变量匹配,包括年龄、性别、术前下肢对齐、术前内侧关节间隙宽度(mJSW)、术前西安大略大学和麦克马斯特大学骨关节炎指数(WOMAC) ) 评分、楔块大小和术后随访时间。通过 WOMAC 问卷评估患者报告的结果,通过 mJSW 评估骨关节炎的放射学进展,以及术前和随访时(> 2 年)的 Kellgren-Lawrence (KL) 分级进展(≥ 1)。失败定义为 HTO 翻修或转为膝关节置换术。
结果
经过倾向评分匹配后,I 组和 II 组包含 58 对患者,A 组和 B 组包含 50 对患者。I、II 组、A、B 组术后 WOMAC 评分及手术失败率差异均无统计学意义(p > 0.05)。然而,I 组术后 mJSW 显着低于 II 组(3.2 ± 1.6 mm vs 3.9 ± 1.8 mm;p = 0.018),A 组显着低于 B 组(3.0 ± 1.7 mm vs 3.7 ± 1.5 mm;p = 0.040 ) )。I 组的 KL 分级进展率显着高于 II 组(53.4% vs 29.3%;p = 0.008),A 组显着高于 B 组(56.0% vs 28.0%;p = 0.005)。
结论
侧向闭合楔形 HTO 后 KJLO 增加(术后 MPTA ≥ 95.0°)或 MPTA 变化≥ 8.0° 不会对患者报告的结果、骨关节炎的放射学进展或平均 5 年随访的手术生存产生不利影响。
证据级别
三、回顾性队列研究。











































 京公网安备 11010802027423号
京公网安备 11010802027423号