Abstract
Purpose
We aimed to compare the staging efficiency of [68Ga]Ga-DOTATATE and [68Ga]Ga-FAPI PET/CT in nasopharyngeal carcinoma (NPC) patients.
Methods
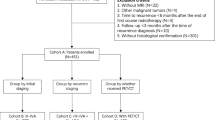
Thirty-nine patients with pathologically confirmed NPC were enrolled in this prospective study. Each patient underwent paired [68Ga]Ga-DOTATATE and [68Ga]Ga-FAPI PET/CT on 2 successive days. The accuracy of two PET/CT for assessing T, N, and M stages was compared by using head-and-neck MRI, histopathologic diagnosis and follow-up results as reference standards. The radiotracer uptake derived from two PETs was also compared.
Results
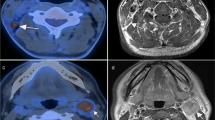
For treatment-naïve patients, [68Ga]Ga-DOTATATE PET/CT showed identical sensitivity for the primary tumours but clearer tumor delineation induced by higher tumour-to-background (TBR) ratio (19.1 ± 8.7 vs. 12.4 ± 7.7, P = 0.003), compared with [68Ga]Ga-FAPI PET/CT. Regarding cervical lymph node (CLN) metastases, [68Ga]Ga-DOTATATE PET had significantly better sensitivity and accuracy based on neck sides (98% vs. 82%, P < 0.001; 99% vs. 88% P = 0.008), neck levels (98% vs. 78%, 99% vs. 97%; both P < 0.001) and individual nodes (89% vs. 56%, 91% vs. 76%; both P < 0.001), and higher TBR (8.1 ± 4.1 vs. 6.3 ± 3.7, P < 0.001). Additionally, [68Ga]Ga-DOTATATE PET/CT revealed higher sensitivity and accuracy for distant metastases (96% vs. 53%, 95% vs. 52%; both P < 0.001), particularly in bone metastases (99% vs. 49%, 97% vs. 49%; both P < 0.001). For post-treatment patients, [68Ga]Ga-DOTATATE PET/CT identified one more true-negative case than [68Ga]Ga-FAPI PET/CT.
Conclusion
[68Ga]Ga-DOTATATE PET/CT performed better than [68Ga]Ga-FAPI PET/CT in visualizing the primary tumours, detecting the metastatic lesions and identifying the local recurrence, suggesting [68Ga]Ga-DOTATATE PET/CT may be superior to [68Ga]Ga-FAPI PET/CT for NPC staging.




Similar content being viewed by others
References
Chen YP, Chan ATC, Le QT, Blanchard P, Sun Y, Ma J. Nasopharyngeal carcinoma. Lancet. 2019;394:394. https://doi.org/10.1016/S0140-6736(19)30956-0.
Hudgins PA, Baugnon KL. Head and Neck: Skull Base Imaging. Neurosurgery. 2018;82:255–67. https://doi.org/10.1093/neuros/nyx492.
Tang LL, Chen WQ, Xue WQ, He YQ, Zheng RS, Zeng YX, et al. Global trends in incidence and mortality of nasopharyngeal carcinoma. Cancer Lett. 2016;374:22–30. https://doi.org/10.1016/j.canlet.2016.01.040.
Young LS, Dawson CW. Epstein-Barr virus and nasopharyngeal carcinoma. Chin J Cancer. 2014; 33: 581 − 90. https://doi:10.5732/cjc.014.10197.
Lee AWM, Ng WT, Chan JYW, Corry J, Mäkitie A, Mendenhall WM et al. Management of locally recurrent nasopharyngeal carcinoma. Cancer Treat Rev. 2019;79:101890. https://doi.org/10. 1016/j. ctrv. 2019. 101890.
Lai V, Khong PL. Updates on MR imaging and 18F-FDG PET/CT imaging in nasopharyngeal carcinoma. Oral Oncol. 2014;50(6):539–48. https://doi.org/10.1016/j.oraloncology.2013.05.005.
Lee SH, Huh SH, Jin SM, Rho YS, Yoon DY, Park CH. Diagnostic value of only 18F-fluorodeocyglucose positron emission tomography/computed tomography-positive lymph nodes in head and neck squamous cell carcinoma. Otolaryngol Head Neck Surg. 2012;147:692–8. https://doi.org/10.1177/0194599812443040.
Tsai MC, Shu YC, Hsu CC, Lin CK, Lee JC, Chu YH, et al. False positive finding of retropharyngeal lymph node recurrence in both fluorine (18)FDG PET and MRI in a patient with nasopharyngeal carcinoma. Head Neck. 2016;38:E84–6. https://doi.org/10.1002/hed.24205.
Tang LL, Chen YP, Chen CB, Chen MY, Chen NY, Chen XZ, The Chinese Society of Clinical Oncology (CSCO) clinical guidelines for the diagnosis and treatment of nasopharyngeal carcinoma.Cancer Commun (Lond), 2021;41:1195 − 227. https://doi:10.1002/cac2.12218.
OuYang PY, Liu ZQ, Lin QG, He Y, Guo ZX, Yao WY, et al. Benefit of [18F] FDG PET/CT in the diagnosis and salvage treatment of recurrent nasopharyngeal carcinoma. Eur J Nucl Med Mol Imaging. 2023;50:881 − 91. https://doi:10.1007/s00259-022-06020-3.
Comoretto M, Balestreri L, Borsatti E, Cimitan M, Franchin G, Lise M. Detection and restaging of residual and/or recurrent nasopharyngeal carcinoma after chemotherapy and radiation therapy: comparison of MR imaging and FDG PET/CT. Radiology. 2008;249:203 − 11. https://doi:10.1148/radiol.2491071753.
Qin C, Liu F, Huang J, Ruan W, Liu Q, Gai Y, et al. A head-to-head comparison of 68Ga-DOTA-FAPI-04 and 18F-FDG PET/MR in patients with nasopharyngeal carcinoma: a prospective study. Eur J Nucl Med Mol Imaging. 2021;48:3228-37. https://doi:10.1007/s00259-021-05255-w.
Zhao L, Pang Y, Zheng H, Han C, Gu J, Sun L, et al. Clinical utility of [68Ga]Ga-labeled fbroblast activation protein inhibitor (FAPI) positron emission tomography/computed tomography for primary staging and recurrence detection in nasopharyngeal carcinoma. Eur J Nucl Med Mol Imaging. 2021;48:3606-17. https://doi:10.1007/s00259-021-05336-w.
Zheng J, Liu F, Lin K, Zhang L, Huang N, Zheng W, et al. [68Ga]GaFAPI PET/CT improves the T staging of patients with newly diagnosed nasopharyngeal carcinoma: a comparison with [18F]FFDG. Mol Imaging Biol. 2022;24:973–85. https://doi.org/10.1007/s11307-022-01748-8.
Loh KS, Waser B, Tan LK, Ruan RS, Stauffer E, Reubi JC. Somatostatin receptors in nasopharyngeal carcinoma. Virchows Arch. 2002;441:444–8. https://doi.org/10.1007/s00428-002-0693-y.
Schartinger VH, Dudás J, Url C, Reinold S, Virgolini IJ, Kroiss A, et al. (68)Ga-DOTA (0)-Tyr (3)-octreotide positron emission tomography in nasopharyngeal carcinoma. Eur J Nucl Med Mol Imaging. 2015;42:20–4. https://doi.org/10.1007/s00259-014-2905-5.
Khor LK, Loi HY, Sinha AK, Tong KT, Goh BC, Loh KS, et al. (68)Ga-DOTA-peptide: a novel molecular biomarker for nasopharyngeal carcinoma. Head Neck. 2016;38:E76–80. https://doi.org/10.1002/hed.24164.
Bennink RJ, van der Meulen FW, Freling NJ, Booij J. Somatostatin receptor scintigraphy in nasopharyngeal carcinoma. Clin Nucl Med. 2008;33:558–61. https://doi.org/10.1097/RLU.0b013e31817dec00.
Zhao L, Pang Y, Wang Y, Chen J, Zhuang Y, Zhang J, et al. Somatostatin receptor imaging with [68Ga]GaDOTATATE Positron emission tomography/computed tomography (PET/CT) in patients with nasopharyngeal carcinoma. Eur J Nucl Med Mol Imaging. 2022;49:1360–73. https://doi.org/10.1007/s00259-021-05587-7.
Lin Z, Zhu W, Zhang J, Miao W, Yao S, Huo L. Head-to-Head comparison of 68Ga-NODAGA-JR11 and 68Ga-DOTATATE PET/CT in patients with metastatic, well-differentiated neuroendocrine tumors: interim analysis of a prospective Bicenter Study. J Nucl Med. 2023;64:1406–11. https://doi.org/10.2967/jnumed.122.264890.
Puré E, Blomberg R. Pro-tumorigenic roles of fbroblast activation protein in cancer: back to the basics. Oncogene. 2018;37:4343–57. https://doi.org/10.1038/s41388-018-0275-3.
Wu HB, Wang QS, Wang MF, Zhen X, Zhou WL, Li HS. Preliminary study of 11 C-choline PET/CT for T staging of locally advanced nasopharyngeal carcinoma: comparison with 18F-FDG PET/CT. J Nucl Med. 2011;52:341–6. https://doi.org/10.2967/jnumed.110.081190.
van den Brekel MW, Stel HV, Castelijns JA, Nauta JJ, van der Waal I, Valk J, et al. Cervical lymph node metastasis: assessment of radiologic criteria. Radiology. 1990;177:379–84. https://doi.org/10.1148/radiology.177.2.2217772.
Zhang GY, Liu LZ, Wei WH, Deng YM, Li YZ, Liu XW. Radiologic criteria of retropharyngeal lymph node metastasis in nasopharyngeal carcinoma treated with radiation therapy. Radiology. 2010;255:605–12. https://doi.org/10.1148/radiol.10090289.
Grégoire V, Ang K, Budach W, Grau C, Hamoir M, Langendijk JA, et al. Delineation of the neck node levels for head and neck tumors: a 2013 update. DAHANCA, EORTC, HKNPCSG, NCIC CTG, NCRI, RTOG, TROG consensus guidelines. Radiother Oncol. 2014;110:172–81. https://doi.org/10.1016/j.radonc.2013.10.010.
Henry LR, Lee HO, Lee JS, Klein-Szanto A, Watts P, Ross EA, et al. Clinical implications of fibroblast activation protein in patients with colon cancer. Clin Cancer Res. 2007;13:1736–41. https://doi.org/10.1158/1078-0432.CCR-06-1746.
Leibel SA, Fuks Z, Zelefsky MJ, Wolden SL, Rosenzweig KE, Alektiar KM, et al. Intensity-modulated radiotherapy. Cancer J. 2002;8:164–76. https://doi.org/10.1097/00130404-200203000-00010.
Lee AW, Ng WT, Pan JJ, Poh SS, Ahn YC, AlHussain H, et al. International guideline for the delineation of the clinical target volumes (CTV) for nasopharyngeal carcinoma. Radiother Oncol. 2018;126:25–36. https://doi:10.1016/j.radonc.2017.10.032.
Li C, Yang Y, Hu F, Xu Y, Wu B, Huang J, et al. Evaluation of 11C-Choline PET/CT for T Staging and Tumor Volume Delineation in Nasopharyngeal Cancer Patients in Comparison to 18F-FDG PET/CT. Clin Nucl Med. 2023;48:563 − 73. https://doi:10.1097/RLU.0000000000004645.
Zaidi H, El Naqa I. PET-guided delineation of radiation therapy treatmentvolumes: a survey of image segmentation techniques. Eur J Nucl Med Mol Imaging. 2010;37:2165-87. https://doi:10.1007/s00259-010-1423-3.
Yang SS, Wu YS, Chen WC, Zhang J, Xiao SM, Zhang BY, et al. Benefit of [18F]-FDG PET/CT for treatment-naïve nasopharyngeal carcinoma. Eur J Nucl Med Mol Imaging. 2022;49:980 − 91. https://doi:10.1007/s00259-021-05540-8.
Qin C, Song Y, Liu X, Gai Y, Liu Q, Ruan W, et al. Increased uptake of 68Ga-DOTA-FAPI-04 in bones and joints: metastases and beyond. Eur J Nucl Med Mol Imaging. 2022;49:709 − 20. https://doi:10.1007/s00259-021-05472-3.
Tang W, Wang Q, Yang S, Chen Y. Elevated 68Ga-FAPI activity in the Plasmacytoma of the ribs. Clin Nucl Med. 2021;46:523–4. https://doi.org/10.1097/RLU.0000000000003632.
Tang W, Wang Q, Yang S, Chen Y. 68Ga-FAPI outperforms 18F-FDG PET/CT in identifying bone metastasis and peritoneal carcinomatosis in a patient with metastatic breast cancer. Clin Nucl Med. 2020;45:913–5. https://doi.org/10.1097/RLU.0000000000003263.
Sun XS, Liu LT, Liu SL, Guo SS, Wen YF, Xie HJ, et al. Identifying optimal candidates for local treatment of the primary tumor among patients with de novo metastatic nasopharyngeal carcinoma: a retrospective cohort study based on EpsteinBarr virus DNA level and tumor response to palliative chemotherapy. BMC Cancer. 2019;19:92. https://doi.org/10.1186/s12885-019-5281-5.
Zou X, You R, Liu H, He YX, Xie GF, Xie ZH, et al. Establishment and validation of M1 stage subdivisions for de novo metastatic nasopharyngeal carcinoma to better predict prognosis and guide treatment. Eur J Cancer. 2017;77:117–26. https://doi.org/10.1016/j.ejca.2017.02.029.
Meng K, Tey J, Ho FCH, Asim H, Cheo T. Utility of magnetic resonance imaging in determining treatment response and local recurrence in nasopharyngeal carcinoma treated curatively. BMC Cancer. 2020;20:193. https://doi.org/10.1186/s12885-020-6664-3.
Straub JM, New J, Hamilton CD, Lominska C, Shnayder Y, Thomas SM. Radiation-induced fibrosis: mechanisms and implications for therapy. J Cancer Res Clin Oncol. 2015;141:1985–94. https://doi.org/10.1007/s00432-015-1974-6.
Zhu W, Zhang J, Singh A, Kulkarni HR, Baum RP. Metastatic nasopharyngeal carcinoma treated with intraarterial combined with intravenous peptide receptor radionuclide therapy. Clin Nucl Med. 2019;44:989–90. https://doi.org/10.1097/RLU.0000000000002788.
Fu K, Pang Y, Zhao L, Lin L, Wu H, Sun L, et al. FAP-targeted radionuclide therapy with [177Lu]Lu-FAPI-46 in metastatic nasopharyngeal carcinoma. Eur J Nucl Med Mol Imaging. 2022;49:1767–9. https://doi.org/10.1007/s00259-021-05634-3.
Funding
This study was supported in part by the Joint Funds for the Innovation of Science and Technology Fujian Province (No.2021Y9134), Natural Science Foundation of Fujian Province (No.2023J01564) and the Fujian Provincial Health Technology Project (No.2022QNA032).
Author information
Authors and Affiliations
Contributions
Experimental design: Jieling Zheng and Weibing Miao; Patients recruiting: Jieling Zheng, Li Su, Wenlong Lv, Chunlin Ke, Peirong Wang, Xiaohui Liu, Feng Liu; Radiopharmaceutical preparation: Yun Yang; PET imaging analyses: Jieling Zheng and Weibing Miao; Immunohistochemistry analysis: Qian Ru and Li Zhang; Statistical analyses: Jieling Zheng and Guochang Wang; Manuscript writing: Jieling Zheng; Manuscript revision: Guochang Wang and Weibing Miao. All authors have seen and approved the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Ethical approval
All procedures involving human participants were carried out in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. This article does not contain any experiments with animals.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zheng, J., Wang, G., Ru, Q. et al. A head-to-head comparison of [68Ga]Ga-DOTATATE and [68Ga]Ga-FAPI PET/CT in patients with nasopharyngeal carcinoma: a single-center, prospective study. Eur J Nucl Med Mol Imaging (2024). https://doi.org/10.1007/s00259-024-06744-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00259-024-06744-4